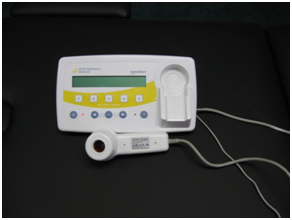
Laser, Cold laser, LED, low-level laser, high power laser, light emitting diode and light therapy are recently gaining popularity in use, although they have been in existence for years. In an effort to meet a demand and see for ourselves the capability of this machine, we have purchased a GaA Super-Pulsed Laser, Infrared Light Emitting Diodes, Red Light Emitting Diodes applicators.
Laser output from our device is as much as 25W (25,000mw) at 905 nm, infrared at 875 nm and red at 660 nm.
We offer a free trial of this technology with a physical therapy evaluation (for those suited to care with this device), as well as the opportunity for continued treatment.
Click here for a video on Laser Therapy
Background on Laser, cold laser, LED, light therapy, IR, red, LLLT, phototherapy, super luminous diode (SLD), super pulsed laser.
Low-energy lasers (also known as cold lasers or class III lasers) have been promoted as an effective way to produce analgesia and accelerate healing of a variety of clinical conditions. The research is good supporting light therapy works well in wound healing. The research is currently more limited in the support for healing for deeper structures.
By definition, low energy laser therapy uses irradiation intensities that induce minimal temperature elevation (not more than 0.1-0.5°C), if any. For practical purposes, this restricts treatment energies to a few J/cm2 and laser powers to 500 mW or less.
Aetna has the following to say about the current research:
Although the results from large, uncontrolled, open trials of low-energy lasers in inducing wound healing have shown benefit, controlled trials have shown little or no benefit. The analgesic effects of low-energy lasers have been most intensely studied in rheumatoid arthritis. Recent well-designed, controlled studies have found no benefit from low energy lasers in relieving pain in rheumatoid arthritis or other musculoskeletal conditions. Furthermore, although positive effects were found in some earlier studies, it was not clear that the pain relief achieved was large enough to have either clinical significance or to replace conventional therapies.
Published systematic reviews of the evidence have concluded that there is a lack of adequate evidence of effectiveness of cold laser therapy for treatment of chronic wounds (e.g., Schneider and Hailey, 1999; Cullum and Petherick, 2007; Flemming and Cullum, 1999; Samson et al, 2004; Simon et al, 2004; Wang, 2004; Nelson and Jones, 2006), arthritis (Brosseau et al, 2007; Brosseau et al, 2005; Marks and de Palma, 1999; Puett and Griffin, 1994; Wang, 2004), tuberculosis (Vlassov et al, 2006; Ziganshina and Garner, 2005), tinnitus (Waddell, 2004), pain (Gross et al, 1998; van der Heijden et al, 2002; Binder, 2002; Speed, 2006; Green et al, 2003), smoking cessation (White et al, 2006), epicondylitis (Chapell, et al., 2002), Achilles tendinitis (McLauchlan et al, 2001), plantar heel pain (Crawford and Thomson, 2003; Landorf and Menz, 2007), back pain (Yousefi-Nooraie, et al., 2008), and other musculoskeletal disorders (de Bie et al, 1998; Abdulwadud, 2001; Ohio BWC, 2004; Wang, 2004). Systematic evidence reviews have also concluded that low-energy laser therapy (e.g., Microlight 830, Microlight Corporation of America, Missouri City, TX) is ineffective in treating carpal tunnel syndrome (Gerritsen et al, 2002; O’Connor et al, 2003; Ohio BWC, 2004; Wang, 2004; CTAF, 2006).
A recent study (Hirschl et al, 2004) evaluated the effectiveness of low-level laser therapy in patients with primary Raynaud’s phenomenon (n = 48). Laser and sham therapy each were applied 5 days a week for 3 weeks. The authors found that low-level laser therapy reduced the frequency and severity of Raynaud attacks. The findings of this study are interesting but need to be validated by further investigation with more patients and follow-up.
Kreisler et al (2004) assessed the effect of low-level laser application on post-operative pain after endodontic surgery in a double-blind, randomized clinical study. Fifty-two healthy adults undergoing endodontic surgery were included into the study. After suturing, 26 patients had the operation site treated with an 809 nm-GaAlAs-laser at a power output of 50 mW and an irradiation time of 150 s. Laser treatment was simulated in another 26 patients. Patients were instructed to evaluate their post-operative pain on 7 days following surgery by means of a visual analogue scale. The results revealed that the pain level in the laser-treated group was lower than in the placebo group throughout the 7 day follow-up period. The differences, however, were significant only on the first post-operative day. The authors stated that low-level laser therapy can be beneficial for the reduction of post-operative pain. However, its clinical effectiveness and applicability with regard to endodontic surgery need further investigation, especially in terms of the optimal energy dosage and the number of laser treatments needed after surgery.
In a randomized controlled study, Bingol et al (2005) examined the effect of low-power gallium-arsenide laser treatment on the patients with shoulder pain. A total of 40 patients with shoulder pain and complied with the selection criteria were included in the study. They were randomly assigned into 2 groups: (i) laser treatment (n = 20), and (ii) control (n = 20). In group (i), patients were given laser treatment and an exercise protocol for 10 sessions during a period of 2 weeks. In group (ii), placebo laser and the same exercise protocol was given for the same period. Patients were evaluated according to the parameters of pain, palpation sensitivity, algometric sensitivity, and shoulder joint range of motion before and after treatment. Analysis of measurement results within each group showed a significant post-treatment improvement for some active and passive movements in both groups, and also for algometric sensitivity in group (i) (p < 0.05 to 0.01). Post-treatment palpation sensitivity values showed improvement in 17 patients (85%) for group (i) and 6 patients (30%) for group (ii). Comparison between two groups showed superior results (p < 0.01 and p < 0.001) in group (i) for the parameters of passive extension and palpation sensitivity but no significant difference for other parameters. These researchers concluded that this study have shown better results in palpation sensitivity and passive extension, but no significant improvement in pain, active range of motion, and algometric sensitivity in laser treatment group compared to the control group in the patients with shoulder pain.
Markovic and Todorovic (2007) compared the effectiveness of dexamethasone and low-power laser (LPL) after surgical removal of impacted lower third molars under local anesthesia (2 % lidocaine / epinephrine). A total of 120 healthy patients were divided into 4 groups of 30 each: (i) group 1 received LPL irradiation immediately after operation (energy output 4 J/cm2 with constant power density of 50 mW, wavelength 637 nm); (ii) group 2 also received intramuscular (i.m.) injection of 4 mg dexamethasone (Dexason) into the internal pterygoid muscle; (iii) group 3 received LPL irradiation supplemented by systemic dexamethasone, 4 mg i.m. in the deltoid region, followed by 4 mg of dexamethasone intra-orally 6 hours post-operatively; and (iv) control group received only the usual post-operative recommendations (i.e., cold packs, soft diet, etc.). LPL irradiation with local use of dexamethasone (group 2) resulted in a statistically significant reduction of post-operative edema in comparison to the other groups. No adverse effects of the procedure or medication were observed. The authors concluded that low-power laser irradiation after lower third molar surgery can be recommended to minimize swelling. The effect is enhanced by simultaneous local intramuscular use of dexamethasone. The drawbacks of this study were two-fold: (i) the effects of low-power laser, if any, was confounded by the simultaneous use of dexamethasone, and (ii) while the combination of low-power laser and dexamethasone achieved a statistical significant reduction in edema, its clinical benefit is unclear.
Stergioulas (2007) compared the effectiveness of a protocol of combination of laser with plyometric exercises and a protocol of placebo laser with the same program, in the treatment of tennis elbow. A total of 50 patients were randomized into two groups: (i) group A (n = 25) was treated with a 904 nm Ga-As laser, frequency 50 Hz, intensity 40 mW and energy density 2.4 J/cm(2), plus plyometric exercises, and (ii) group B (n = 25) that received placebo laser plus the same plyometric exercises. During 8 weeks of therapy, patients of the two groups received 12 sessions of laser or placebo, 2 sessions per week (weeks 1 to 4) and 1 session per week (weeks 5 to 8). Pain at rest, at palpation on the lateral epicondyle, during resisted wrist extension, middle finger test, and strength testing was evaluated using visual analog scale. Also, the grip strength, the range of motion and weight test were evaluated. Parameters were determined before treatment, at the end of the 8th week course of treatment (week 8), and 8th (week 8 ) after the end of treatment. Relative to group B, group A had (i) a significant decrease of pain at rest at the end of 8 weeks of the treatment (p < 0.005) and at the end of following up period (p < 0.05), (ii) a significant decrease in pain at palpation and pain on isometric testing at 8 weeks of treatment (p < 0.05), and at 8 weeks follow-up (p < 0.001), (iii) a significant decrease in pain during middle finger test at the end of 8 weeks of treatment (p < 0.01), and at the end of the follow-up period (p < 0.05), (iv) a significant decrease of pain during grip strength testing at 8 weeks of treatment (p < 0.05), and at 8 weeks follow-up (p < 0.001), (v) a significant increase in the wrist range of motion at 8 weeks follow-up (p < 0.01), (vi) an increase in grip strength at 8 weeks of treatment (p < 0.05) and at 8 weeks follow-up (p < 0.01), and (vii) a significant increase in weight-test at 8 weeks of treatment (p < 0.05) and at 8 weeks follow-up (p < 0.005). The authors concluded that these findings suggested that the combination of laser with plyometric exercises was more effective treatment than placebo laser with the same plyometric exercises at the end of the treatment as well as at the follow-up. Moreover, they stated that future studies are needed to establish the relative and absolute effectiveness of the above protocol.
Kaviani and colleagues (2006) examined the effects of low level laser therapy (LLLT) in the treatment of post-mastectomy lymphedema. A total of 11 women with unilateral post-mastectomy lymphedema were enrolled in a double-blind controlled trial. Patients were randomly assigned to laser and sham groups and received laser or placebo irradiation (Ga-As laser device with a wavelength of 890 nm and fluence of 1.5 J/cm2) over the arm and axillary areas. Changes in patients’ limb circumference, pain score, range of motion, heaviness of the affected limb, and desire to continue the treatment were measured before the treatment and at follow-up sessions (weeks 3, 9, 12, 18, and 22) and were compared to pre-treatment values. Results showed that of the 11 enrolled patients, 8 completed the treatment sessions. Reduction in limb circumference was detected in both groups, although it was more pronounced in the laser group up to the end of 22nd week. Desire to continue treatment at each session and baseline score in the laser group was greater than in the sham group in all sessions. Pain reduction in the laser group was more than in the sham group except for the weeks 3 and 9. No substantial differences were seen in other two parameters between the two treatment groups. The authors concluded that despite the encouraging results, further studies of the effects of LLLT in management of post-mastectomy lymphedema should be undertaken to determine the optimal physiological and physical parameters to obtain the most effective clinical response.
In a systematic review of common conservative therapies for arm lymphoedema secondary to breast cancer treatment, Moseley et al (2007) stated that secondary arm lymphoedema is a chronic and distressing condition which affects a significant number of women who undergo breast cancer treatment. A number of health professional and patient instigated conservative therapies have been developed to help with this condition, but their comparative benefits are not clearly known. This systematic review undertook a broad investigation of commonly instigated conservative therapies for secondary arm lymphoedema including; complex physical therapy, manual lymphatic drainage, pneumatic pumps, oral pharmaceuticals, LLLT, compression bandaging and garments, limb exercises and limb elevation. It was found that the more intensive and health professional based therapies, such as complex physical therapy, manual lymphatic drainage, pneumatic pump and laser therapy generally yielded the greater volume reductions, whilst self-instigated therapies such as compression garment wear, exercises and limb elevation yielded smaller reductions. All conservative therapies produced improvements in subjective arm symptoms and quality of life issues, where these were measured. Despite the identified benefits, there is still the need for large scale, high level clinical trials in this area.
Information on lymphedema from the BC Cancer Agency (2007) notes that laser therapy “may or may not work but need[s] further study.”
High-power lasers (class IV therapeutic lasers; not to be confused with class IV surgical lasers) have power output of up to 7,500 mW; and supposedly offer more power, deeper penetration (can penetrate up to 10 cm2 instead of 0.5 to 2.0 cm2 for class III lasers) and a larger surface treatment area (cover up to 77 cm2 instead of 0.3 to 5.0 cm2 for class III lasers). Despite little scientific support, high-power lasers have been employed for various indications including musculoskeletal disorders (e.g., carpal tunnel syndrome and lateral epicondylitis), pain relief, and wound healing. Plaghki and Mouraux (2005) noted that laser heat stimulators selectively activate Adelta and C-nociceptors in the superficial layers of the skin. Their high-power output produces steep heating ramps, which improve synchronization of afferent volleys and thus allow the recording of time-locked events (e.g., laser-evoked brain potentials). Study of the electrical brain activity evoked by Adelta- and C-nociceptor afferent volleys revealed the existence of an extensive, sequentially activated, cortical network. These electro-physiological responses are modulated by stimulus-driven and, even more extensively, top-down processes. The specificity and validity of these components for pain research are currently under intense scrutiny.
In a systematic review on treatment of pressure ulcers, Reddy and colleagues (2008) concluded that there is little evidence to support routine nutritional supplementation or adjunctive therapies including laser therapy compared with standard care.
Carrasco et al (2009) noted that limited studies have demonstrated that LLLT may have a therapeutic effect on the treatment of myofascial pain syndrome (MPS). In this study, 60 patients with MPS and having one active trigger point in the anterior masseter and anterior temporal muscles were selected and assigned randomly to 6 groups (n = 10 in each group): Groups I to Ill were treated with GaAIAS (780 nm) laser, applied in continuous mode and in a meticulous way, twice weekly, for 4 weeks. Energy was set to 25 J/cm2, 60 J/cm2 and 105 J/cm2, respectively. Groups IV to VI were treated with placebo applications, simulating the same parameters as the treated groups. Pain scores were assessed just before, then immediately after the 4th application, immediately after the 8th application, at 15 days and 1 month following treatment. A significant pain reduction was observed over time (p < 0.001). The analgesic effect of the LLLT was similar to the placebo groups. The authors stated that using the parameters described in this experiment, LLLT was effective in reducing pain experienced by patients with MPS. Thus, it was not possible to establish a treatment protocol.
Yelden and colleagues (2009) examined the effectiveness LLLT in addition to exercise program on shoulder function in subacromial impingement syndrome (SAIS). A total of 67 patients with SAIS were randomly assigned to either a group that received laser (n = 34) or a group that received placebo laser (n = 26). Pain, functional assessment, disability and muscle strength of shoulder were assessed before and after a 3-week rehabilitation program. Besides laser or placebo laser, superficial cold and progressive exercise program were administered to both groups, 5 days a week, for 3 weeks. A progressive exercise program that was done twice daily under supervision in clinic and at home was given to the patients. After the treatment, all outcome measurements had shown significant improvement except muscle strength in both the groups. When the parameters of the improvement were compared, there were no significant differences between the two groups after treatment. The authors concluded that there is no fundamental difference between LLLT and placebo LLLT when they are supplementing an exercise program for rehabilitation of patients with shoulder impingement syndrome.
In a prospective, randomized double-blind study, Teggi et al (2009) examined the effectiveness of LLLT for tinnitus. A total of 60 outpatients with tinnitus presenting sensorineural hearing loss in the affected ear were included in the study. They were randomly divided into 2 groups: (i) active laser therapy 20 mins a day for 3 months with a 650-nm, 5-mW soft laser (group L), and (ii) control group with dummy device, which duplicated all aspects of active laser therapy except for the activation of the laser beam. One subject in both groups dropped out due to an increase in tinnitus loudness. Two more patients in each group ceased to comply with the protocol due to familiar problems. Main outcome measure was the Tinnitus Handicap Inventory (THI); no statistical difference was detected between the 2 groups in the THI total score (p = 0.97), and its functional (p = 0.89), emotional (p = 0.89) and catastrophic (p = 0.89) subscales. Moreover, a visual analog scale for self-perceived loudness of the tinnitus showed no difference between the groups (p = 0.69). Regarding psychoacoustic parameters, the minimum masking level showed no difference (p = 0.42), while loudness expressed in sensation level exhibited lower values in the treatment group (p = 0.0127). Subjects in the treatment group also reported a decreased rate of hyper-acusis (p = 0.02). No changes were detected in the audiometric threshold in both groups. The authors concluded that soft laser therapy demonstrated no efficacy as a therapeutic measure for tinnitus.
A systematic evidence review by Chow, et al. (2009) concluded that low-level laser therapy reduced pain immediately after treatment in acute neck pain, and up to 22 weeks after completion of treatment, in patients with chronic neck pain. The authors included randomized controlled clinical trials (RCTs) or quasi-RCTs of low-level laser therapy, for participants aged 16 or over with acute or chronic neck pain, were eligible for inclusion. Sixteen RCTs (n=820 participants) met inclusion criteria, with sample sizes ranging from 20 to 90 participants. The authors reported significant effects of low level laser therapy on acute and chronic neck pain. An evaluation of the systematic evidence review by Chow, et al. by the Centre for Reviews and Dissemination (2009) found that, although suitable methods were employed to reduce the risks of reviewer error and bias for the processes of study selection and data extraction, the authors did not report on whether such methods were used to assess study quality, which was assessed using the Jadad scale. The CRD also found that this did not assess methods of allocation concealment, so the risk on investigator bias affecting trial results could not be ruled out. Furthermore, no information was provided on the actual levels of withdrawals and drop-outs. The CRD also found that all trials included in this systematic review had relatively small sample sizes and information was not provided on whether treatment groups (in individual trials) were comparable at baseline for likely confounders. The CRD noted that the authors of the systematic review acknowledged the considerable clinical heterogeneity in laser treatment parameters, but this also seemed apparent with regard to the sites treated, diagnoses, frequencies of treatment, and uses of cointerventions; it is therefore questionable whether meta-analysis was the most appropriate method of synthesis. The CRD concluded: “Although many aspects of this review were well-conducted, the considerable clinical heterogeneity seen, coupled with uncertainty regarding possible bias in the small trials included, mean the authors’ conclusions should be interpreted with a degree of caution.”



Recent Comments